Decentralized and Hybrid Clinical Trials: Models, Tools, and Best Practices
The world of clinical trials is evolving fast. And, pivoting this transformation are decentralized and hybrid clinical trial models. The two approaches are redefining how research is conducted by shifting the focus toward flexibility, efficiency, and patient-centricity. With the market for decentralized clinical trials expected to grow from $9.63 billion in 2024 to over $21 billion by 2030; this shift is driving healthtech towards full-scale modernization.
Today's trials are becoming more inclusive and accessible, driven by digital health technologies like mobile apps, telemedicine, and wearable devices. These tools enable real-time data collection, remote monitoring, and continuous patient engagement; while reducing the logistical and financial burdens associated with traditional site-based models. With decentralized trials are hybrid models that are emerging as the preferred approach for many sponsors. It is a blend of the best of both worlds: remote participation and in-person visits. As we explore the tools and best practices behind these models, one thing is clear: decentralized and hybrid trials have graduated from being experimental to aggressively shaping the future of clinical research.
What Is a Decentralized Clinical Trial (DCT)?
As decentralized and hybrid models reshape the clinical trial landscape, it is important to understand what exactly a decentralized clinical trial (DCT) entails. A DCT shifts many aspects of a traditional site-based trial into the patient’s own environment. It could be their home or a local healthcare facility. DCTs bring the trial to the participant patients with the help of digital tools for remote participation.
DCTs are often referred to as “virtual trials” or “direct-to-participant” studies. They rely on technologies like telemedicine, wearable devices, mobile health apps, and remote monitoring platforms to collect and manage data. Patients may consult with investigators via video calls, receive study medications at home, and even perform certain assessments themselves. Digital biomarkers collected through wearables offer continuous insights into patient health, while secure cloud-based systems manage trial data in real time.
A fully decentralized trial may involve no physical contact between the patient and the study team at all. However, many current trials adopt a hybrid approach that retains certain in-person procedures while decentralizing others.
Key features of DCTs include:
- Telemedicine for virtual consultations
- E-consent to streamline enrollment
- Home-based assessments for convenience
- Digital tools to track patient health in real time
- Centralized data systems for secure data handling
- Digital data capture via ePRO, eCOA, and EDC systems
Ultimately, DCTs represent a fundamental shift toward patient-centric research; thus, bringing more comfort, flexibility, and accessibility to clinical trial participation.
What Is a Hybrid Clinical Trial?
While fully decentralized clinical trials have unlocked new levels of convenience and accessibility, they are not always the right fit for every study. A complete traditional trial, or a complete DCT might not answer the needs of many. Therefore, Hybrid clinical trials present a model that strikes a balance between virtual participation and traditional site-based elements.
In a hybrid trial, certain activities like initial screenings, lab tests, or complex procedures, still take place at clinical sites. But much of the day-to-day monitoring, such as symptom tracking or vital sign measurement, is handled remotely using tools like mobile apps, wearable sensors, or remote patient monitoring (RPM) platforms. This mix allows patients to stay engaged from the comfort of their homes without sacrificing the safety or accuracy that in-person touchpoints provide.
Hybrid trials have advantages that score over the other two approaches. They reduce the number of required site visits, making participation more manageable for people with busy schedules, mobility issues, or chronic health conditions. At the same time, sponsors retain opportunities for face-to-face interaction.
Real-time data from wearables like ECG patches and biosensors is funneled into centralized dashboards, giving research teams continuous insight into patient status. Even if a patient misses a visit, data collection does not stop. This flexible, tech-enabled approach helps improve recruitment, retention, and the overall quality of the research. Hybrid clinical trials translate into scientific rigor paired with modern convenience.
Core Technologies Enabling DCTs
Building on the flexibility offered by hybrid models, fully decentralized clinical trials can push the boundaries further, with the intervention of digital health technologies. This is largely due to mobile apps, telehealth platforms, and wearable devices. These tools not only reduce the burden on participants but also enable richer, more continuous data collection. Patients can now report symptoms like pain in real time through virtual platforms installed on their smartphones. This immediate, patient-reported input brings researchers closer to real-world evidence than ever before.
Bluetooth-enabled wearables and sensors capture metrics such as oxygen saturation, ECG, or EEG data. These data are fed directly into secure cloud-based systems, minimizing delays and manual errors. Telehealth visits and home healthcare services replace many site-based interactions, further decentralizing the trial process without sacrificing data integrity or patient safety.
One of the newest technologies gaining ground is automated electronic patient-reported outcomes (ePRO). With the ability to capture images, audio, and video, these tools reduce subjectivity and standardize reporting, offering deeper insights into the patient experience.
By leveraging these integrated technologies, DCTs are smarter, faster, and closer to real life than traditional trials.
Successful decentralized and hybrid trials rely on an integrated digital ecosystem. Core technologies include:
- eConsent and remote enrollment platforms that guide participants through eligibility and consent without requiring site visits
- EDC (Electronic Data Capture) systems for managing structured trial data
- ePRO/eCOA tools for capturing patient-reported and clinician-reported outcomes
- Telehealth platforms to conduct video visits, assessments, and safety monitoring
- Home health and mobile nursing services for at-home sample collection and exams
- Wearables and connected devices that collect real-time health data
- EHR integration to pull in real-world data for screening or outcome tracking
DCT Operational Models
With technology having become the backbone of decentralized clinical trials (DCTs), how these trials are operationalized can vary based on the level of decentralization, oversight, and patient engagement required. Broadly, there are three main operational models: fully remote, hybrid, and site-led vs. sponsor-led DCTs.
A fully remote DCT takes decentralization to its fullest extent. In this model, all trial-related activities; recruitment, eConsent, monitoring, and data collection, happen remotely. Participants never need to visit a traditional site; instead, they engage from their homes using tools like telemedicine, mobile apps, and wearables. This model is highly patient-centric, removing travel barriers and offering greater flexibility, often leading to improved recruitment and retention.
Hybrid DCTs, as discussed earlier, combine the best of both virtual and physical worlds. While routine monitoring and reporting can happen remotely, key procedures like lab tests or imaging might still occur at clinical sites. The challenge lies in harmonizing both components that ensure tech adoption, data quality, and regulatory compliance without disrupting the patient experience.
DCTs can also differ in leadership structure. Site-led trials rely on local investigators to manage patient interactions and data capture, while sponsor-led trials are coordinated centrally by the sponsor or CRO. The former boosts patient trust through local relationships; the latter enables tighter control over timelines, data integrity, and protocol adherence. Selecting the right operational model is key to aligning trial goals with patient needs and technological readiness.
Regulatory and Ethical Considerations
As operational models shift toward hybrid and fully decentralized designs, one thing remains unchanged: DCTs must still meet the same ethical and regulatory standards as traditional clinical trials. However, the way those standards are applied needs to adapt to new tools, workflows, and participant experiences.
Regulatory bodies like the FDA have issued specific guidance around decentralized trials, telehealth, and the use of digital health tools. Parallely, Institutional Review Boards (IRBs) now review eConsent workflows, virtual procedures, and remote monitoring strategies with a renewed lens. Ensuring informed consent validation that includes identity verification and comprehension checks is paramount in remote settings, where face-to-face interactions are limited.
Data privacy regulations, such as HIPAA in the U.S. and GDPR in the EU, also take center stage. With sensitive health data collected and transmitted via mobile apps and wearable devices, robust privacy, security, and audit mechanisms must be in place from the start.
To navigate this evolving landscape, sponsors must work closely with legal, compliance, and ethics teams during trial design and deployment. Key ethical concerns also include ensuring equitable access to digital tools, maintaining patient safety remotely, and preventing participant isolation.
Ultimately, a proactive, cross-functional approach is essential. By embedding regulatory and ethical safeguards into the foundation of DCTs, sponsors can build flexible trials that are efficient, inclusive, compliant and trustworthy.
Best Practices for Designing a Decentralized or Hybrid Trial
With regulatory and ethical frameworks steadily evolving to support decentralized and hybrid clinical trials, the next step is to chalk out a thoughtful, strategic design. While DCTs are not entirely new, today’s technology platforms have transformed how effectively they can be managed to make it easier to reduce site burden, improve patient engagement, and deliver high-quality data at scale.
A successful DCT starts with patient-centric design. Understanding the needs, preferences, and limitations of your target population is essential. Involving patients early - through surveys or advisory boards, helps shape trial protocols that are not only accessible but intuitive. Every digital touchpoint should be seamless and user-friendly to minimize friction and keep participants engaged.
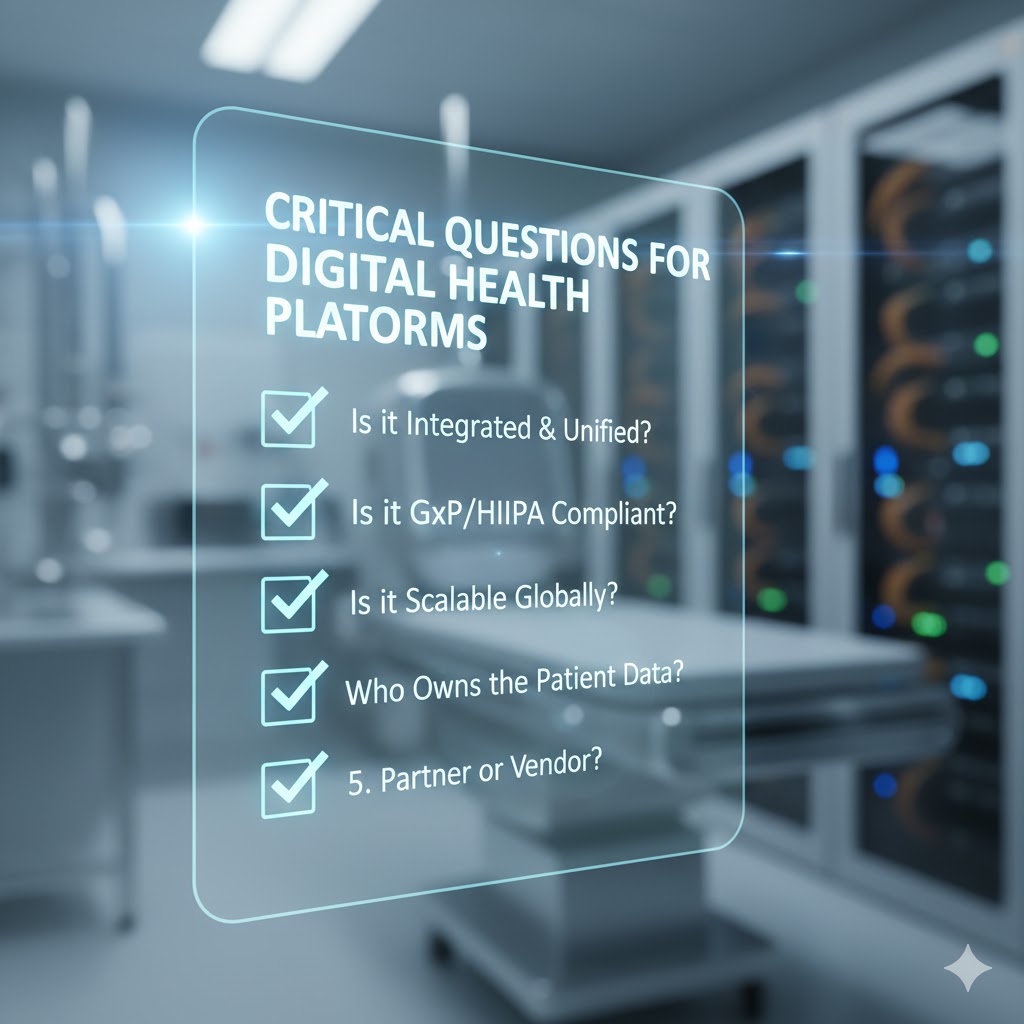
Equally important is technology selection and integration. Choose interoperable platforms that can scale. This starts with essentials like eConsent, and evolves to include ePRO, telehealth, and wearables as needed. Devices should be comfortable, unobtrusive, and reliable, while all tools must adhere to strict data security standards.
Data management and regulatory compliance are non-negotiable. A robust plan for data collection, validation, and security ensures data integrity and meets global privacy requirements like HIPAA and GDPR.
Lastly, invest in training and support for both staff and participants, and maintain oversight through remote monitoring systems and regular audits.
By aligning stakeholder needs and following these best practices, sponsors can design DCTs that are flexible, efficient, and truly patient-first.
Common Pitfalls to Avoid
Even with best practices in place, decentralized and hybrid clinical trials can falter if key challenges are overlooked during planning and execution. After designing a thoughtful, patient-centric model with the right technology and oversight, the next step is avoiding common missteps that can undermine trial success.
One major pitfall is overcomplicating the tech stack. Using too many disconnected digital tools can create confusion for both patients and site staff, leading to data silos and inconsistent workflows. Instead, aim for an integrated platform that simplifies the experience while maintaining data quality.
Another risk is neglecting digital literacy. Not every participant will be equally comfortable with mobile apps, wearables, or telemedicine. Failing to provide clear guidance or technical support can cause frustration, reduce compliance, and increase dropout rates.
Skipping a pilot phase is another common error. Pilot testing is essential to validate usability, assess workflow feasibility, and uncover potential roadblocks before full-scale deployment.
In hybrid trials, underestimating site coordination can also lead to inefficiencies. Sites need clear roles, proper training, and active communication channels to manage both in-person and remote components seamlessly.
Careful planning, proactive stakeholder involvement, and early-stage testing can help avoid these pitfalls. It can help ensure that your decentralized or hybrid trial runs smoothly, keeps patients engaged, and delivers robust, reliable results.
Case Examples and Real-World Scenarios
The impact of well-designed hybrid and decentralized clinical trials is being proven practically. Sponsors are seeing tangible benefits through clinical trials that are delivering results:
In one Phase 2 oncology trial, transitioning from a traditional to a hybrid model significantly reduced dropout rates by enabling telehealth for follow-up visits thus, giving patients flexibility without compromising care.
A rare disease registry leveraged at-home sample collection and a mobile app to reach participants in remote areas. It successfully expanded enrollment and improved data diversity.
Meanwhile, a medical device trial adopted a fully decentralized model, using eConsent, wearables, and electronic data capture (EDC). The result was a 40% reduction in data lock time. It streamlined the trial’s timeline without sacrificing data integrity.
These examples highlight the practical value of hybrid and decentralized models particularly, when thoughtfully designed, they deliver better outcomes for patients, researchers, and sponsors alike.
Key Takeaways
With an analysis of real-world examples we reach the end where we come to the conclusion that decentralized and hybrid clinical trials are redefining how research is done. These approaches are expanding access, increasing efficiency, and improving patient satisfaction by meeting participants where they are.
However, there is no one-size-fits-all model. The success of a DCT or hybrid trial hinges on flexibility, thoughtful design, and alignment with both scientific objectives and patient needs. From technology selection to stakeholder coordination, every decision must serve the larger goal of smarter, more inclusive research.
It is also important to remember that technology is an enabler and not a solution in itself. Tools like telemedicine, wearables, and eConsent platforms only add value when they are a part of a well-integrated, patient-centric strategy.
With the right planning and execution, decentralized and hybrid trials can drive better outcomes for patients, sponsors, and the future of clinical research.
Frequently Asked Questions (FAQs)
1. What’s the difference between decentralized and virtual trials?
Virtual trials are typically fully remote and digital, conducted without in-person site visits. Decentralized clinical trials (DCTs), however, combine both digital tools and physical locations. They offer flexibility by using telehealth, home visits, or local labs—providing a hybrid model that improves accessibility while maintaining essential in-person interactions when needed.
2. Can you use sites in a decentralized trial?
Yes, decentralized trials often incorporate physical sites alongside remote technologies. Many DCTs use a hybrid approach, combining in-person visits at clinical sites with virtual tools like ePRO, telemedicine, or home health services. This allows for greater participant flexibility while maintaining clinical oversight where necessary.
3. Are DCTs suitable for all trial phases?
Decentralized trials are most commonly used in Phase 2 and 3 studies, where patient engagement and data collection are critical. However, their adoption is expanding into early-phase trials and post-market studies as technology improves and regulatory frameworks become more supportive of remote and hybrid research models.
4. How are participants onboarded remotely?
Participants are onboarded remotely through digital tools such as eConsent platforms, telehealth consultations, and user-friendly onboarding workflows. These systems provide step-by-step guidance, verify eligibility, and ensure patients understand the trial process—allowing for a smooth, compliant, and patient-centric entry into decentralized or virtual clinical trials.